Guide to Pulse Oximetry
Pulse oximeters have revolutionized anesthesia monitoring because of their ease of use, rapidity of application,
reliability as continuous, peripheral pulse monitors and their ability to non-invasively measure hemoglobin
(Hb) saturation with O2 (SpO2). Pulse oximeters can detect problems in two main areas. First is hypoxia (lack
of oxygen delivery to tissue), which is the most common cause of anesthetic mortality; second is changes in
pulse strength and regularity - commonly caused by lack of blood flow, bradycardia, and dysrhythmias.
Basic Understanding
1. Physiology
2. Methodology

Physiology
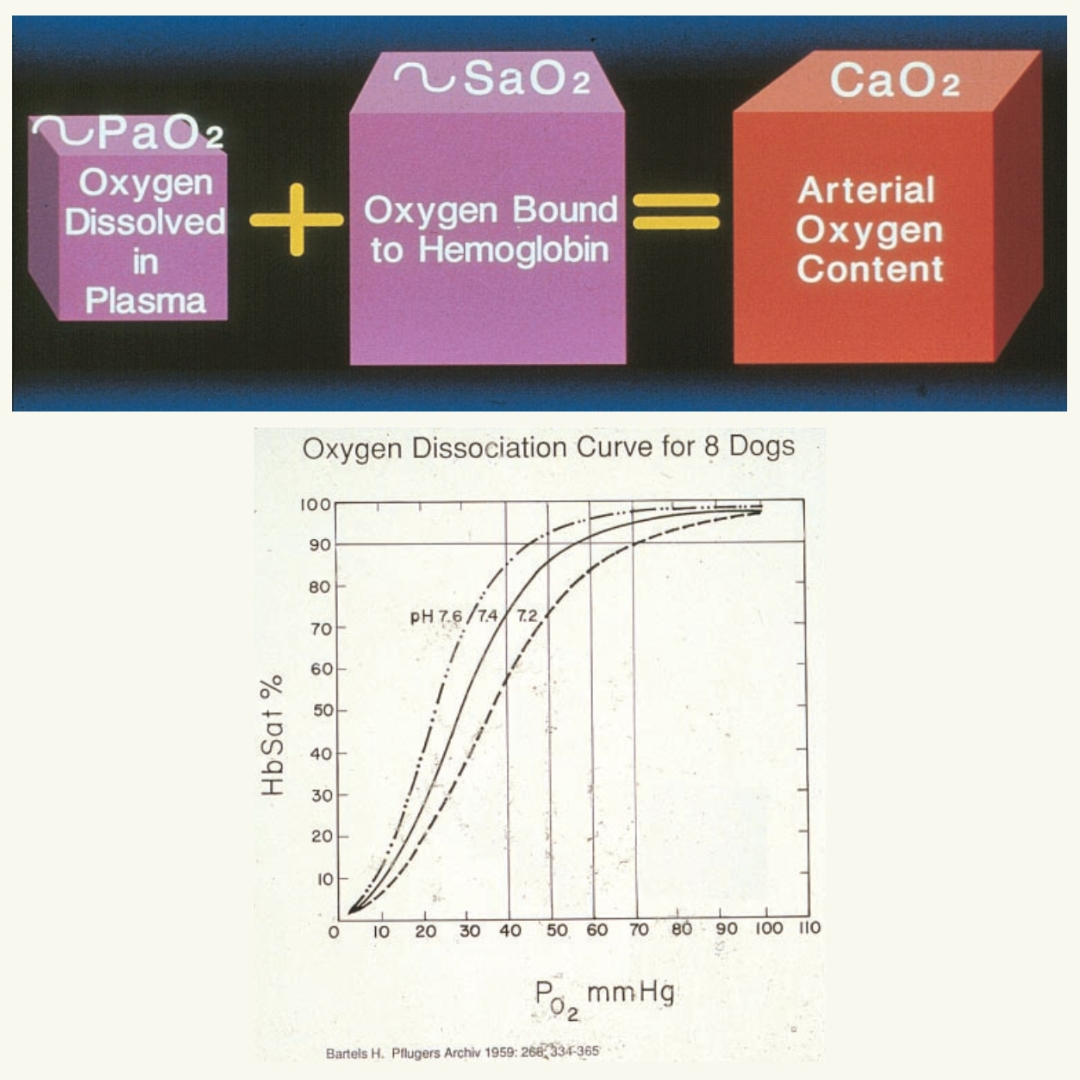
- Tissue O2 Delivery = Blood Flow x Content of O2
- Blood O2 Content = Hb concentration x SpO2 dissolved in plasma
- Over 97% of the O2 is carried on hemoglobin (Hb). Halving the PCV (40 to 20) halves the blood O2 content but SpO2 won’t change!
- O2 binds to Hb in a sigmoidal relationship so arterial blood SaO2 should be over 90% to stay above the steep decline on this curve, corresponding to a PO2 > 60 to 65 mm Hg in dogs. Venous blood SvO2 is typically 70 to 85%
Methodology
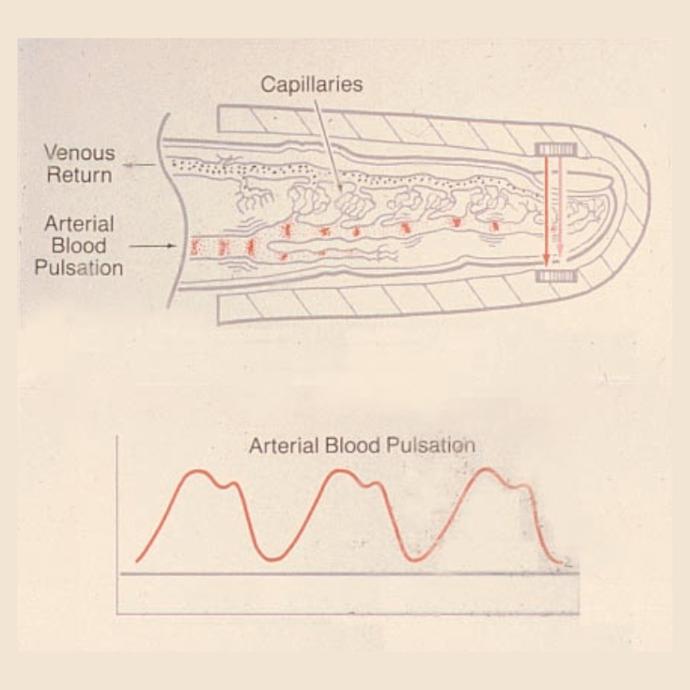
- Pulse oximetry is the continuous non-invasive monitoring of peripheral capillary bed SpO2 via absorption of infrared light.
- The absorption characteristics of hemoglobin vary with oxygen saturation.
- The infrared light must be transmitted through skin or mucosa, subcutaneous tissue, bone, and the blood volume filling the capillary bed (the total sum of which = "background absorption") as well as the arterial pulsatile blood volume (used to determine SpO2).
- Pulse oximeter SpO2 readings decrease because of low Hb O2 saturation (hypoxemia) or the background light absorption changes (lower blood flow).
SpO2 Interpretation and Trouble Shooting
Sensors application sites
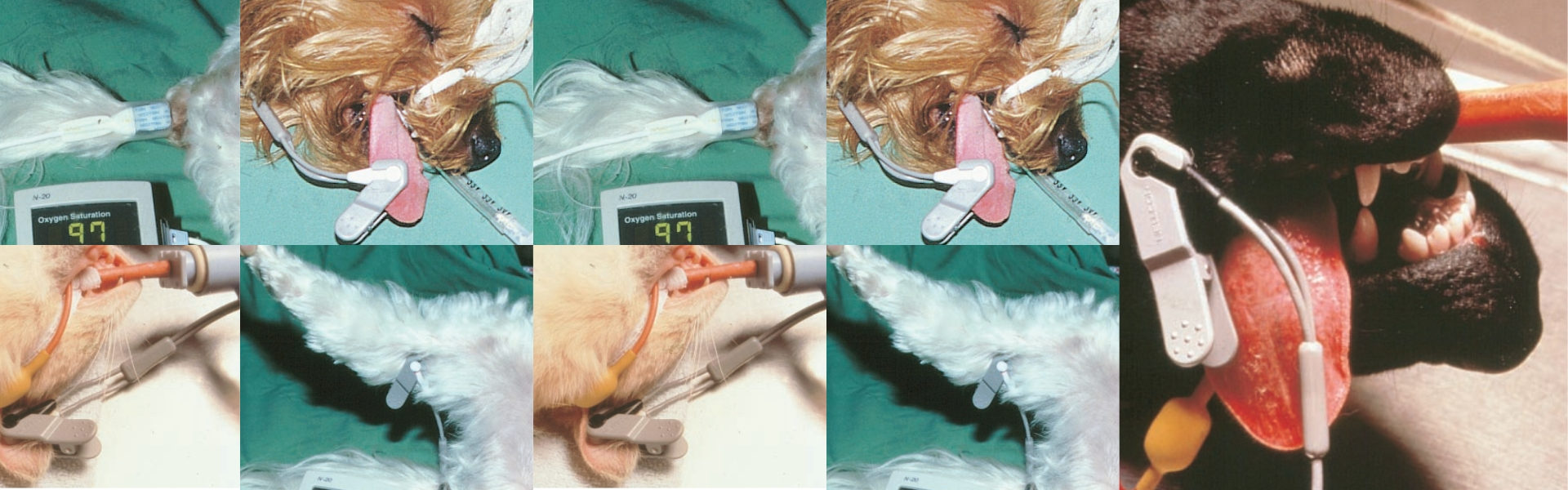
The most useful sites for application of clip-type sensors in dogs & cats are the tongue, the lip, and the ear in non-pigmented skin. Other
useful sites include the paw of cats, across the individual toes of dogs, and the thin skin fold above the hock caudal to the tibia. Clipping a
small area of hair at the application site (e.g. ear, hock) will improve sensor performance.
Handle tissue (tongue, ear, etc) gently when positioning sensors to avoid vasoconstriction which alters SpO2 readings. In cats and other
small patients, folding a surgical swab over the tongue underneath the probe improves performance because this eliminates some
light, “damping the signal.” Motion artifacts (sensor movement or shivering) and extraneous light reduce pulse oximeter performance.
Dark, pigmented skin absorbs most of the infrared light so pulse oximetry won’t work.
Interpretation of SpO2 readings
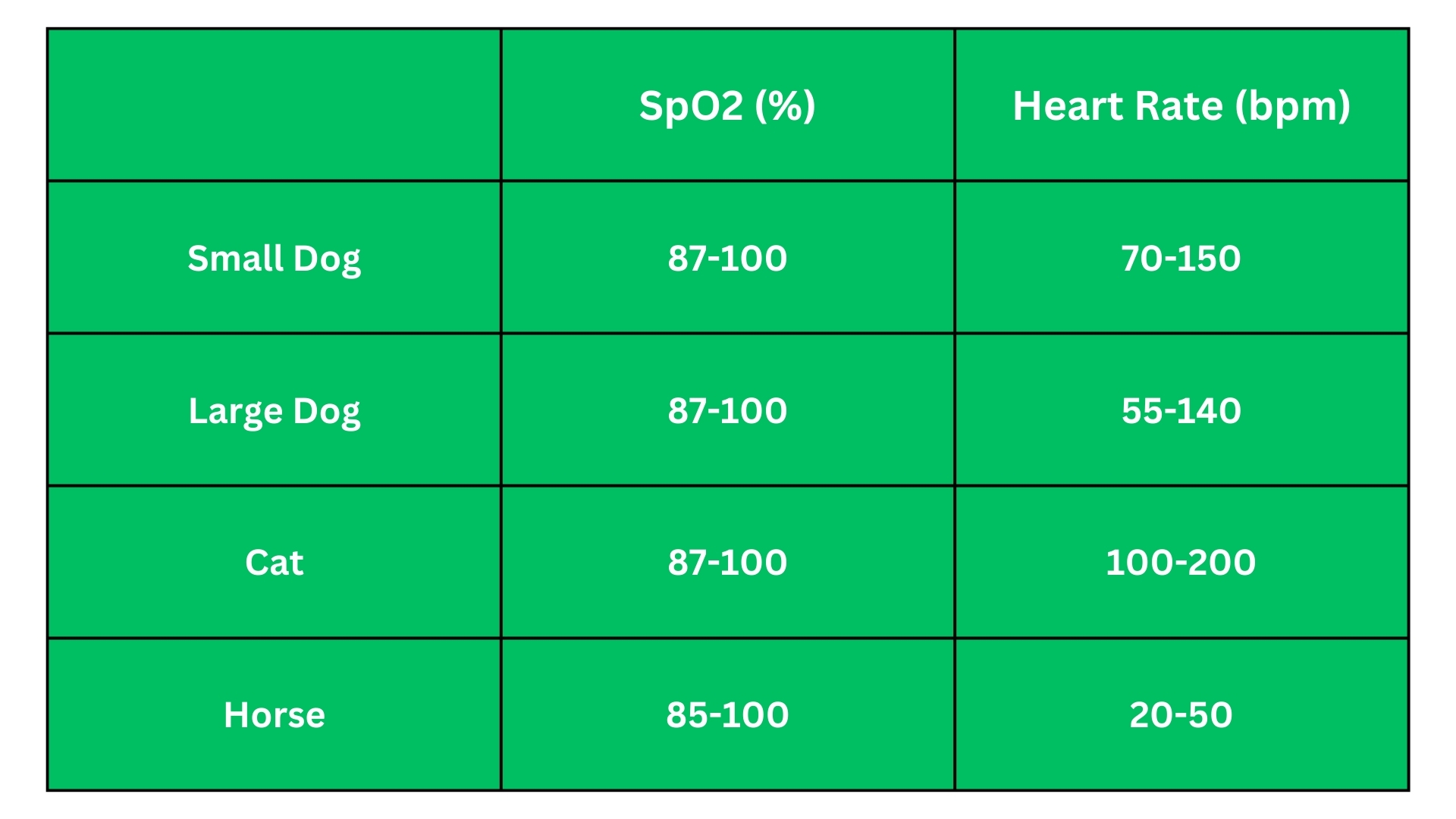
SpO2 and pulse rate normal ranges measured with pulse oximeters
Alarm Settings
SpO2 measured by a pulse oximeter is generally 2-3% lower than SaO2 because it reads capillary blood through skin/mucosa. We aim to maintain arterial Hb O2 over 90% so alarms are typically set at 85% to 87%.
Troubleshooting low SpO2 readings
1. Look at the Patient
- Is there a pulse?
- Is there breathing?
- What is the mucous membrane color?
- What is happening in surgery? (e.g. pain causes vasoconstriction)
2. Problem management Low Perfusion
- Decrease in capillary blood volume (flow) altering background light absorption
- Vasoconstriction from painful stimulation - consider anesthesia
- Poor perfusion caused by deep anesthesia
- Decrease anesthesia
- Increase IV fluids
- Consider inotropes (e.g. dopamine or dobutamine)
- Reposition the sensor if there are no signs of hypoxia (below). This will cause the monitor to "re-set" itself using the new blood flow so the SpO2 reading should improve to what it was prior to the change
3. Problem management - Hypoxia

- Poor pulmonary dysfunction
- Signs of hypoxia: cyanosis, high HR & RR
- ensure adequate ventilation: minimum I breath/30 sec (O2 95%)
- Increase inspired oxygen level
- Improve pulmonary blood flow

- PCV below 15-20% consider transfusion
- O2 by mask
- Tight fitting
- 95% from anesthesia breathing circuits
- Flow 100 to 200 ml/kg/min
- Improve pulmonary blood flow